Bleeding Peptic Ulcer: Treatment
A peptic ulcer is an open sore in the lining of your stomach (called a gastric ulcer) or duodenum (the first part of the small intestine). Your ulcer is bleeding or at high risk of bleeding. This means that you need treatment right away. Treatment can include medicines. It may also include a procedure such as endoscopy, angiography, or surgery. Your provider will work with you to decide which treatments are best for you.
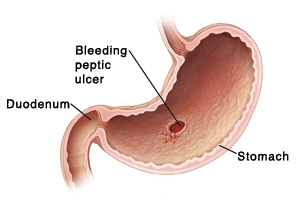 |
| A bleeding peptic ulcer is a serious problem and must be treated right away. |
Treatment with medicines
Medicines will be prescribed as part of your treatment. Combinations of medicines are needed. These can include:
-
Antibiotics. These medicines kill the H. pylori (Helicobacter pylori) bacteria if it's present. An H. pylori infection is the most common cause of a peptic ulcer. You will have to take several antibiotics at the same time.
-
Proton pump inhibitors. These block your stomach from making any acid.
-
H2 blockers. These reduce the amount of acid your stomach makes.
-
Bismuth subsalicylate. This helps kill H pylori along with other medicines.
When taking medicines, be aware of the following:
-
Each medicine has risks and side effects. Your healthcare provider will tell you more about these, based on the medicines that are prescribed for you.
-
Treatment with antibiotics lasts about 7 to 14 days. You may need to take other types of medicines for a longer time. Be sure to take all of the medicines exactly as instructed. Don’t stop taking the medicines even if you are feeling better.
-
During treatment, don't take nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin and ibuprofen. Overuse of these medicines is another possible cause of ulcers. Using them can make your symptoms worse. If you take aspirin or blood thinners (anticoagulants) because of a heart condition, blood clot, or stroke, talk with your healthcare provider first before you stop taking them. Your provider can best determine which medicines to continue and which to stop.
-
Your provider may also advise you to not have cigarettes, alcohol, or caffeine. These may make your symptoms worse. They may also affect how well your ulcer heals.
Treatment with endoscopy, interventional angiography, or surgery
Along with medicines, your treatment may include endoscopy, interventional angiography, or surgery. Endoscopy is usually the first treatment used. Here’s what to expect with each treatment:
Before the treatment
During the treatment
A needle is placed in a vein in your hand or arm. It’s attached to an IV (intravenous) line. The IV line gives you fluids. It also gives you medicine to prevent pain. This may include medicine to make you drowsy (sedative) or sleep (anesthesia) during treatment. The provider will then treat your ulcer with one of the following:
-
Endoscopy. This procedure uses a thin, flexible tube called an endoscope (scope). The scope has a tiny camera on the end. This lets the provider find the ulcer. First, your throat may be numbed with a spray or gargle. Then, the scope is put into your mouth and guided down into your stomach or duodenum. Air is used to expand the digestive tract. Once the ulcer is found, tiny tools are passed through the scope to stop any bleeding. These may include clips or devices that use heat or electricity. In some cases, medicine (epinephrine) is injected directly into the ulcer to help reduce bleeding. When the bleeding is stopped, the air is removed. The scope and any tools used are then also removed.
-
Interventional angiography. A long catheter is threaded into the arteries near the ulcer. A coil, absorbable sponge, or medicine is put into the blood vessel to stop the ulcer bleeding.
-
Surgery. This can be done in two different ways:
-
Open surgery. A cut (incision) is made in your belly (abdomen) to reach the ulcer. This lets the surgeon see and treat the ulcer directly.
-
Laparoscopy. A few small cuts are made in your belly. A scope with a tiny camera is then inserted through one of the cuts. Pictures of the inside of your belly are sent to a screen. This lets the provider find the ulcer. Tiny tools are then passed through the other cuts to treat the ulcer. Nearby nerves, blood vessels, and parts of the stomach may also be treated. Once the surgery is done, any tools used are removed and the cuts are closed.
After the treatment
You’ll be taken to the PACU (post-anesthesia recovery unit) or ICU (intensive care unit). Nurses will watch your condition closely. You’ll be moved to a hospital room when you’re stable. You will be given medicines to help manage pain and to ease symptoms. Tests may be done to see if your ulcer is bleeding again. You’ll stay in the hospital until your provider confirms there are no problems.
Before leaving the hospital, make sure you have all the prescriptions and home care instructions you’ll need. Also make sure you have a contact number for your provider or the hospital. This is in case you have problems or questions after treatment.
New types of treatment are also being studied. Ask your provider about any new treatment options.
Risks and possible complications of treatment
For endoscopy:
-
Bleeding
-
A hole (perforation) in your upper digestive tract (this includes your esophagus, stomach, and duodenum)
-
Risk of reactions to sedation medicines or anesthesia used
-
The ulcer coming back
For angiography:
For surgery:
-
Bleeding
-
Infection
-
Damage to nearby organs and blood vessels
-
Long-term digestive problems such as irregular bowel movements
-
Risks of reactions to anesthesia
-
The ulcer coming back
-
Death
Follow-up
Keep all follow-up appointments with your provider. These are needed to check your health and recovery progress.
When to call your healthcare provider
Call your healthcare provider right away if you have any of the following:
-
Trouble breathing or chest pain (call 911)
-
Fever of 100.4° F ( 38°C) or higher, or as advised by your healthcare provider
-
Increased redness, pain, swelling, bleeding, or drainage from any incisions
-
Trouble swallowing or sore throat that doesn’t go away within 2 days
-
Belly pain that won’t go away
-
Black, tarry, or bloody stools
-
Upset stomach (nausea) and vomiting
Online Medical Reviewer:
Jen Lehrer MD
Online Medical Reviewer:
Raymond Kent Turley BSN MSN RN
Online Medical Reviewer:
Rita Sather RN
Date Last Reviewed:
2/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.