Painful Menstrual Periods (Dysmenorrhea)
Dysmenorrhea is the term used to describe painful menstrual periods.
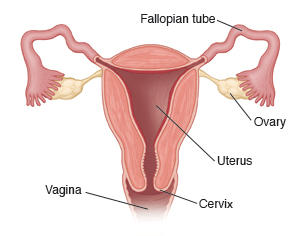
The uterus is a muscle. Normally, chemicals called prostaglandins cause the uterus to contract during your period. The contractions push out the buildup of tissue that occurs each month inside the uterus. If the contraction is very strong, it can cause pain. The pain may feel like cramping in the lower belly (abdomen), lower back, or thighs. In severe cases, you may have other symptoms as well. These can include nausea, vomiting, loose stools, sweating, or dizziness.
There are two types of dysmenorrhea:
Primary dysmenorrhea. This is common menstrual cramps. It may begin 1 or 2 years after you first get your period. It may get better or go away as you get older or when you have a baby. The cramps are most often felt just before, or on the first day of your period. They may last 1 to 3 days. It is treated with medicines and comfort measures as described below (see the Home care section).
Secondary dysmenorrhea. This may start later in life. It describes menstrual pain that occurs due to an underlying health problem. The pain may last longer than common menstrual cramps. It may also get worse over time. Some problems that can lead to secondary dysmenorrhea include:
-
Pelvic inflammatory disease (PID). Infection that involves the female reproductive organs, such as the uterus and fallopian tubes.
-
Fibroids. Noncancer (benign) growths within the wall of the uterus.
-
Endometriosis. Tissue that normally only lines the uterus also grows outside of it (because the abnormal tissue also swells and bleeds each month, it can cause pain).
Once the cause of secondary dysmenorrhea is found, it can be treated. Your healthcare provider will discuss options with you as needed. Your care may also include some of the treatments described below (see the “Home care” section).
Home care
Medicines
Certain medicines can help ease or prevent menstrual pain and cramping. These can include:
-
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen
-
Prescription pain medicine, if needed
-
Hormone therapy (this includes most methods of hormonal birth control such as pills, vaginal rings, patches, shots, or a hormone-releasing IUD)
General care
To help ease pain and cramping, try these tips:
-
Rest, as needed.
-
Apply a heating pad to the lower belly or back as directed. A warm bath or massage to these areas may also help.
-
Exercise regularly. Many people find that being more active each week helps reduce pain and cramping.
-
Ask your healthcare provider for advice about other treatments you can try to help control pain and cramping.
Follow-up care
Follow up with your healthcare provider, or as advised.
When to get medical advice
Call your healthcare provider right away if any of these occur:
-
Fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
-
Pain or cramping gets worse or doesn’t get better with medicine
-
Pain or cramping lasts longer than normal or occurs between periods
-
Abnormal vaginal discharge between periods
-
Bleeding becomes heavy (soaking more than 1 pad or tampon every hour for 3 hours)
-
Pink or gray tissue passes from the vagina