Abdominal Aortic Aneurysm (Stable)
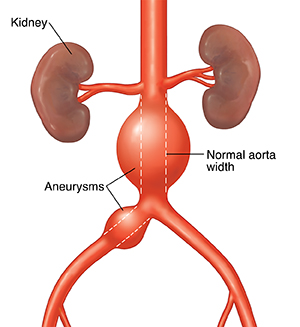
The aorta is the body’s main artery that carries oxygen-rich blood away from the heart. The artery runs from the heart down to the lower belly (abdomen). There it divides into smaller blood vessels.
An aneurysm is a bulge (dilatation) in the wall of an artery. This happens because there is a weak spot in the artery wall causing that area to start to deteriorate. This allows the artery to bulge or balloon out, creating the aneurysm. It may remain stable and cause no problems. Or it can expand and lengthen. If this happens, it can affect the blood flow to different organs. It may also leak or break open (rupture) and cause internal bleeding and even death.
Many things can cause aortic aneurysms including:
-
Hardening of the arteries (atherosclerosis)
-
High blood pressure (hypertension)
-
Injury
-
Infection
-
Marfan syndrome (an inherited condition that most often affects the heart, eyes, blood vessels, and skeleton)
Risk factors that have been linked to aortic aneurysms include:
Most aortic aneurysms don't cause any symptoms until they start to expand rapidly or rupture. Most aneurysms are found during exams or tests, such as an X-ray or CT scan, done for other reasons. When there are symptoms, they may be unclear or hard to feel. They can include:
-
Deep, steady pain in the abdomen and back
-
Pulsating feeling in your abdomen
-
Weakness
-
Dizziness and fainting
-
Low blood pressure
-
Pain, discoloration, or sores on the feet (rare)
Once there are symptoms, it's important to take care of the aneurysm right away. Untreated, an expanding aneurysm causes pain in the belly (abdomen), back, sides (flank), or area between the abdomen and inner thigh (groin). This pain may come and go at first and then become constant. When an aneurysm ruptures, there can be sudden pain in the abdomen, back, or groin. Weakness, dizziness, and loss of consciousness may happen next as blood pressure drops and a state of shock sets in. This condition will lead to death, unless immediate surgery is done.
Small aneurysms rarely rupture. They can often be treated with medicines to lower blood pressure and reduce stress on the aortic wall. Routine ultrasound or CT scans can show if the aneurysm is growing. Larger or expanding aneurysms will need surgery. A surgeon will remove the section of aorta with the aneurysm and replace it with an artificial blood vessel (graft). A newer option can be used in certain cases. It involves the placement of a tubular wire mesh (stent) inside the aorta. The stent supports the wall and reduce stress on the aneurysm. With a stent, there is a rare risk that a blood clot can form inside of the aortic aneurysm without causing any symptoms. A piece of the clot can break off and pass to smaller blood vessels in the intestines or legs, which causes pain and loss of blood flow to that part of the body.
If a small aneurysm has been found, you should change any lifestyle factors that may improve your overall heart and blood vessel health. This may include eating a healthy diet, losing weight, stopping smoking, and lowering your blood pressure and cholesterol.
Home care
-
Your aneurysm is small and may not need surgery. You'll be watched closely and have routine ultrasounds to measure the size of the aneurysm every 6 months to 3 years depending on its size.
-
You may return to your usual level of activity.
-
Follow these guidelines to improve your heart and blood vessel health:
-
If you're overweight, start a weight loss program.
-
If you have high blood pressure, reduce your salt intake. Don't eat high-salt foods or add salt when cooking.
-
Start an exercise program. Talk with your healthcare provider about what type of exercise program is best for you. It doesn't have to be hard. Even brisk walking for 30 minutes 5 times a week is a good form of exercise.
-
Don't take medicines containing stimulants. This includes many cold and sinus decongestant pills and sprays, as well as diet pills. Check the label for warnings about high blood sugar. Stimulants, such as amphetamine or cocaine, could be deadly for someone with high blood pressure. Never take them.
-
Limit your caffeine intake or switch to caffeine-free products.
-
Stop smoking. Ask your provider for help and enroll in a stop-smoking program to improve your chance of success.
-
Learning how to handle stress better is an important part of any program to lower blood pressure. Learn about relaxation methods, such as meditation, yoga, and biofeedback.
-
If medicines were prescribed for high blood pressure, take them exactly as directed. Missing doses may cause your blood pressure to get out of control.
-
Consider buying an automatic blood pressure machine, which is available at most pharmacies. Use this to monitor your blood pressure at home. Share the results with your provider.
Follow-up care
Regular visits to your provider for blood pressure checks and ultrasounds of the aorta are an important part of your care. Make a follow-up appointment as advised.
When to get medical advice
Call your provider if any of these occur:
-
Sudden severe pain in the abdomen, back, flank, or groin
-
Blood in your bowel movements (stools)
-
Weakness or dizziness
-
Weakness, numbness, pain, or coolness of one leg
Call 911
The symptoms of a heart attack or stroke can be life-threatening. If you see or have any of these symptoms, call 911 right away:
-
Trouble breathing
-
Confusion or having a hard time waking up
-
Fainting or loss of consciousness
-
Fast heart rate
-
New pain in the chest, arm, shoulder, neck, or upper back
-
Trouble talking or seeing
-
Weakness in 1 arm or leg
-
Trouble walking or loss of balance
-
Numbness or weakness on 1 side of your body
-
Drooping of 1 side of the face