Chlamydia, Treated (Female)
Gendered terms are used here to talk about anatomy and health risk. Please use this information in a way that works best for you and your provider as you talk about your care.
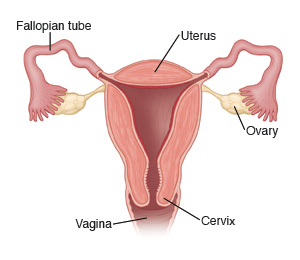
You have an infection called chlamydia. This is a sexually transmitted infection (STI). It may also be called a sexually transmitted disease (STD). It can be passed easily from one person to another. It's passed on by having vaginal, anal, or oral sexual contact with an infected partner. Chlamydia can infect the internal sex organs. These are the cervix, uterus, and fallopian tubes. It can also infect the mouth, throat, and anus. But this happens less often.
Women with an infection in the cervix may have no symptoms. Or they may have only mild symptoms early in the illness. That’s why you are able to pass this infection on without knowing you have it.
When symptoms do occur, they often start 2 to 10 days after you are exposed to chlamydia. You may have a vaginal discharge. You may have pain or burning when you urinate. The infection is called pelvic inflammatory disease (PID) if it spreads to the fallopian tubes. This causes lower belly (abdominal or pelvic) pain and fever. Chlamydia that isn’t treated can make you unable to have children (infertility). This is because it harms the fallopian tubes. PID also makes it more likely for you to have a tubal (ectopic) pregnancy in the future. This is a serious health problem.
Chlamydia can be treated and cured. Treatment is with medicines called antibiotics.
Home care
Follow these guidelines when caring for yourself at home:
-
Your sexual partner must be treated at the same time. This is true even if they have no symptoms. Your partner should reach out to their own healthcare provider for treatment. They can also go to an urgent care clinic or the public health department. Sometimes your own provider may prescribe antibiotics for your partner. This is called expedited partner therapy.
-
Don’t have sex until both you and your partner have finished taking all the antibiotics. Wait until your healthcare provider has told you that you are cured.
-
Take all medicines until they are gone, even if you feel better. Otherwise, your symptoms and the infection may come back.
-
Learn about safe sex practices and use these in the future. The safest sex is with a partner who has tested negative and only has sex with you. Condoms may keep you from spreading some STIs. These include gonorrhea, chlamydia, and HIV. However, condoms are not a guarantee.
-
Talk with your healthcare provider about chlamydia screening. Chlamydia infection is most common in sexually active people 24 or younger. In females, it can cause serious problems like pelvic inflammatory disease, ectopic pregnancy, and infertility. For this reason, yearly screening for chlamydia is recommended for all sexually active females age 24 or younger, and in females age 25 and older who are at risk for infection.
Follow-up care
STI testing
-
Follow up with your healthcare provider on any test results, or as advised. Talk with your provider or your local health department to be sure you are having complete STI (including HIV) screening. Also make sure you are lowering your risk of STIs, including HIV, as much as possible. This includes HIV testing. Call the CDC National STI Hotline at 800-232-4636 or go to the CDC STI website for more information about STIs.
-
People who get chlamydia can get another STI at the same time, such as gonorrhea, syphilis, or HIV. Get tested for HIV now. If negative, get tested again in 3 months. Also talk with your healthcare provider about whether taking anti-HIV medicines would be a good idea. Your provider may advise you to take such medicine now for 28 days or on an ongoing basis to prevent you from getting HIV.
Tell your partner
Make sure you talk with your partner about STIs and testing. If you don't feel safe talking face-to-face with your partner about testing, send a text or email. Or make a phone call instead. Ask for help if you’re not safe. Encourage your partner(s) to get treatment. Otherwise, they can pass the infection back to you or others.
If you have an STI, talk with your healthcare provider about expedited partner therapy (EPT) . With EPT, you may be given a prescription or medicines to give to your partner without your partner needing to be seen by a healthcare provider. EPT is available in many states for some STIs (mainly chlamydia and gonorrhea). Check with your provider.
When to seek medical care
Call your healthcare provider right away if any of the following occur:
-
Symptoms not better after 3 days of treatment
-
New pain in your lower abdomen or back
-
Pain in your lower abdomen or back gets worse
-
Unexpected vaginal bleeding
-
Weakness, dizziness, or fainting
-
Repeated vomiting
-
Unable to urinate because of pain
-
Rash or joint pain
-
Painful open sores around the outer vagina
-
Enlarged, painful lumps (lymph nodes) in your groin
-
Fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider