Kidney Stone, Undescended, No Symptoms
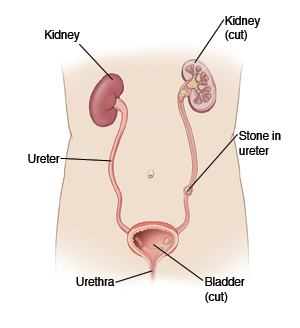
A kidney stone (nephrolithiasis) starts as tiny crystals. They form inside the kidney where urine is made. Most kidney stones enlarge to about 1/8 to 1/4 inch in size before leaving the kidney and moving toward the bladder. There are four types of kidney stones. Eighty percent are calcium stones—mostly calcium oxalate but also some with calcium phosphate. The other three types include uric acid stones, struvite stones (from a preceding infection), and rarely, cystine stones.
When the stone breaks free and starts to move down the ureter (the narrow tube joining the kidney to the bladder) it often causes sharp, severe back and side pain. Nausea and vomiting also often occur. When the stone reaches the bladder, the pain stops. Once in your bladder, the kidney stone may pass through the urethra (urinary opening) while you are urinating (which may cause pain to start again). Or it may break into such small fragments that you don’t notice it passing.
Your kidney stone is still inside the kidney. There is no way to predict how long it will be before it breaks free and causes any symptoms. Most stones will pass on their own within a few hours to a few days (sometimes longer). You may notice a red, pink, or brown color to your urine. This is normal while passing a kidney stone. A large stone may not pass on its own and may require special procedures to remove it. These procedures include:
-
Lithotripsy. This uses ultrasound waves to break up the stone.
-
Ureteroscopy. A thin, basket-like instrument is pushed through the urethra and bladder to pull out the stone.
-
Surgery. This is done directly through the skin.
Home care
These guidelines will help you care for yourself at home:
-
Drink plenty of fluids. This increases urine flow. It also reduces the risk of further stone formation. Healthy adults (no heart/liver/kidney disease) who have had a kidney stone should drink 12 8-ounce glasses of fluids per day. Most of this should be water. The goal is to produce 1.5 to 2 quarts of almost colorless urine per 24 hours.
-
You should collect your urine in a container. Then, drain it through a strainer to collect any stones or pieces of stones. Take these to your healthcare provider to help identify your specific type of stone. This will aid in future treatment and dietary changes.
-
Try to stay as active as possible since this will help the stone pass. Don't stay in bed unless you have pain that prevents you from getting up. As you can tolerate it, try walking short distances, even if it's just around the house.
-
If you develop pain, you may take ibuprofen or naproxen for pain, unless another medicine was prescribed. If you have chronic liver or kidney disease, or ever had a stomach ulcer or gastrointestinal bleeding, talk with your healthcare provider before using these medicines.
Prevention
Each year, there is a 5% to 10% chance that a new stone will form. Over the next 5 to 7 years, there is a 50% chance that a new stone will form. The risk is higher if you have a family history of kidney stones. It is also higher if you have certain chronic illnesses such as high blood pressure, obesity, or diabetes. However, there are lifestyle and dietary changes that you can make to reduce the risk of a recurrence.
Most kidney stones are made of calcium. The following is advice for preventing a recurrence of calcium stones. If you don’t know the type of stone you have, follow this advice until the cause of your stone is determined.
Things that help:
-
The most important thing you can do is to drink plenty of fluids each day, as described above.
-
Certain foods, such as wheat, rice, rye, barley and beans, contain phytate. This is a compound that may lower the risk of recurrence of any type of stone.
-
Eat more fruits and vegetables (especially those high in potassium).
-
Eat foods high in natural citrate like fruit and fruit juices (using low sugar).
-
Low calcium contributes to the formation of calcium type kidney stones. Eat a normal calcium diet and speak with your doctor if you are taking calcium supplements. It may be detrimental to reduce your calcium intake. New research shows that eating calcium-rich and oxalate-rich foods together lowers your risk of stones. This happens by binding the minerals in the stomach and intestines before they can reach the kidneys.
-
Limit salt intake to 2 grams (1 teaspoon) per day. Use limited amounts when cooking. And don’t add salt at the table. Processed and canned foods are usually high in salt.
-
Spinach, rhubarb, peanuts, cashews, almonds, grapefruit, and grapefruit juice are all high-oxalate foods. They should be reduced or eaten with calcium-rich foods. These foods include dairy, dark leafy greens, soy products, and calcium enriched foods.
-
Reducing the amount of animal meat in your diet may lower your risk of uric acid stones.
-
Don't have excess sugar (sucrose) and fructose (sweetener in many soft drinks) in your diet.
-
If you take vitamin C as a supplement, don't take more than 1,000 milligrams (mg) per day.
-
A dietitian or your healthcare provider can provide you with specific details about dietary changes to prevent kidney stone recurrence.
Follow-up care
Follow up with your healthcare provider, or as advised. Talk with your healthcare provider about urine and blood tests to find out the cause of your stone. Write down questions you have about your kidney stones or diet. Bring them with you to your appointments.
If you had an X-ray, CT scan, or other diagnostic test, you will be notified of any findings that may affect your care.
Call 911
Call 911 if you have any of these:
When to seek medical advice
Call your healthcare provider right away if any of these occur:
-
Severe sharp back or side pain
-
Repeated vomiting or unable to keep down fluids
-
Fever of 100.4ºF (38ºC) or higher, or as directed by your healthcare provider
-
Blood (pink or red color) in your urine
-
Foul smelling or cloudy urine
-
Unable to pass urine for 8 hours or increasing bladder pressure
-
New or worsening symptoms