H. Pylori Infection with Peptic Ulcer
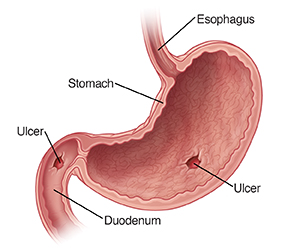
A peptic ulcer is an open sore in the lining of the upper part of the gastrointestinal (GI) tract. It may be present in the stomach (gastric ulcer) or the first part of the small intestine called the duodenum (duodenal ulcer).
Symptoms of a peptic ulcer include stomach pain and upset. Nausea, vomiting, bloating, belching, or bleeding may sometimes occur. The bleeding may be seen as fresh blood in vomit or vomit that looks like coffee grounds. There may be black tarry stools as well.
The 2 most common causes of peptic ulcer are infection with the bacteria called H. pylori and the use of a type of pain medicine called nonsteroidal anti-inflammatory drugs (NSAIDs).
Many people have H. pylori in their bodies. Most of the time, it causes no problems. In some people, though, the H. pylori infection irritates the stomach lining. This may make the lining more likely to be damaged by normal stomach acids. H. pylori may also increase the amount of acid in the stomach. It is not clear why this infection leads to problems in some people and not in others.
NSAIDs, such as aspirin, ibuprofen, and naproxen, can cause peptic ulcers. The risk is higher when they are used for a longer time.. They make the stomach lining more vulnerable to damage and ulcer formation. Other drugs, such as corticosteroids and bisphosphonates, may also cause peptic ulcers.
Tests may be done to check for H. pylori infection. These include a blood test, a breath test, and a stool test. In some cases, a test called endoscopy may be done. During this test, a thin, lighted tube is put into the mouth and down the throat. The healthcare provider can look at the esophagus, stomach, and duodenum through this tube. During this test, a tiny sample of stomach lining (biopsy) may be taken and tested for H. pylori.
Home care
-
Medicines are used to treat H. pylori infection. Two or more medicines are usually taken together for about 2 weeks or more. Treatment depends on the underlying cause of peptic ulcers. Antibiotics may be given if H pylori infection is present.
-
Other medicines include antacids, H2 blockers, proton pump inhibitors and bismuth subsalicylate.
-
If aspirin or other NSAIDs are the cause of ulcers, your healthcare provider may suggest stopping them or changing their dosage. Do not stop any medicines unless your healthcare provider recommends it.
-
Take all prescribed medicines as directed. Take all of the medicines until your healthcare provider asks you to stop. This is very important. If you don't finish the medicines, the infection may remain and may be harder to treat.
-
Ask your healthcare provider what side effects the medicines might cause. These can include stomach cramps, diarrhea, or constipation.
-
After the medicine is finished, you may have another test to see if H. pylori infection is still present.
-
Stay away from alcohol and smoking during treatment.
Follow-up care
Follow up with your healthcare provider as directed. Be sure to return to be retested for H. pylori after treatment.
When to get medical advice
Call your healthcare provider for any of the following:
Call 911
Call 911 if any of the following occur:
-
Vomiting a large amount of blood (dark or bright red)
-
Passing a large amount of blood (dark or bright red) in the stool
-
Chest pain appears, gets worse, or spreads to the back, neck, shoulder, or arm
-
Fainting or loss of consciousness