Canker Sore (Child)
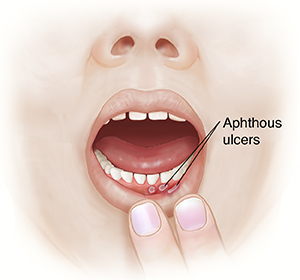
A canker sore is a painful sore on the lining of the mouth. It’s also called an aphthous ulcer. It's most painful during the first few days, and it lasts about 7 to 14 days before going away.
Causes
Canker sores are not cold sores or fever blisters. They are not contagious, so they are not spread by contact. The exact cause of canker sores is not clear. But there are various things that can trigger them in different people:
-
Mild injury, such as biting the inside of the mouth, lip, or cheek, or dental procedures
-
Stress
-
Poor diet, or lack of certain nutrients, including B vitamins and iron
-
Foods that can irritate the mouth, including tomatoes, citrus fruits, and some nuts (foods that are acidic or contain bitter substances called tannins)
-
Irritating chemicals, such as those in some toothpastes and mouthwashes
-
Some chronic illnesses
Symptoms
Canker sores occur on the lining of the mouth. They can be inside the cheeks or lips, on the roof of the mouth, at the base of the gums, on the tongue, or in the back of the throat. Canker sores:
-
Are small and flat (not raised)
-
Can be white or yellowish bumps that are red around the edges or have a red halo around them
-
Are usually small in size, roundish, and in groups
-
Cause pain or burning
Canker sores don't leave a scar. But they usually come back.
Home care
The goals of canker sore treatment are to decrease the pain, speed healing, and prevent sores from coming back. No single treatment works for everyone. Try different methods to see what works best for your child.
Medicines
Your child’s healthcare provider may prescribe a numbing gel to help ease the pain of a canker sore. Follow all instructions for this.
General care
-
Use a clean cloth or tissue to pat the ulcer dry before applying any medicine.
-
Apply the medicine with a clean cotton swab.
-
Be sure your child uses only a soft-bristle toothbrush and brushes the teeth gently.
-
Don't let your child eat foods that can cut or scrape the inside of the mouth, such as potato chips.
-
Don't give your child spicy, salty, or acidic foods such as lemons and tomatoes. These can irritate the sores.
Homemade rinses and solutions
Children may rinse their mouth for 1 minute with either of the following solutions. After rinsing, the solution should be spit out, not swallowed. Another method, which can be used with children who are too young to rinse and spit, is to dab the mixture on the sores with a cotton swab. You can repeat these treatments as often as needed.
-
Rinse the mouth with saltwater (1/2 teaspoon of salt in 1 glass of warm water).
-
Mix equal amounts of hydrogen peroxide and water. This can be used as a mouth rinse or dabbed on sores with a cotton swab. You can also add sodium bicarbonate to this to make a paste, and then dab it on the sores.
Special note to parents
Numbing gels or mouth rinses may sting at first. Reassure your child that this pain lasts just a short time.
Follow-up care
Follow up with your child’s healthcare provider, or as advised. If a culture was done, you can call as directed for the results. You will be told if your child’s treatment needs to be changed.
Call 911
Call 911 if your child has any of these:
When to seek medical advice
For a usually healthy child, call your child's healthcare provider right away if any of these occur:
-
Your child has a fever (see Fever and children, below).
-
Your child has a sore that doesn't heal within 2 weeks.
-
Your child has pain that doesn’t get better or go away.
-
Your child has trouble eating or drinking.
-
Your child has several canker sores in a year.
-
Your child shows signs of infection. These include redness, swelling, or pain that gets worse, or fluid from the canker sore that smells bad.
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use a rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below is when to call the healthcare provider if your child has a fever. Your child’s healthcare provider may give you different numbers. Follow their instructions.
When to call a healthcare provider about your child’s fever
For a baby under 3 months old:
-
First, ask your child’s healthcare provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
-
A fever of ___________as advised by the provider
For a child age 3 months to 36 months (3 years):
-
Rectal or forehead: 102°F (38.9°C) or higher
-
Ear (only for use over age 6 months): 102°F (38.9°C) or higher
-
A fever of ___________ as advised by the provider
In these cases:
-
Armpit temperature of 103°F (39.4°C) or higher in a child of any age
-
Temperature of 104°F (40°C) or higher in a child of any age
-
A fever of ___________ as advised by the provider