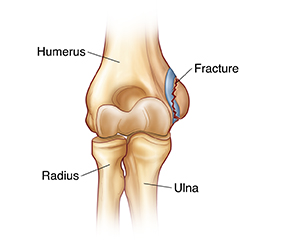
Elbow Fracture (Child)
Your child has a fracture (broken bone) in the elbow. An elbow fracture often causes pain, swelling, and bruising. The elbow may also look odd-shaped. The elbow joint is composed of 3 bones. The humerus is the bone in the upper arm and it attaches to the radius and ulna, the 2 bones of the lower arm. An elbow fracture can occur in any of these bones, but the most common is in the humerus.
X-rays are usually the first test done to diagnose an elbow fracture. Small fractures may be hard to see in children, so additional follow-up X-rays may be needed to confirm the injury. If a fracture is suspected, a splint is typically applied to keep the bones from moving. If the fracture is severe, it may be necessary to try to realign the bones before placing a splint or cast. Many elbow fractures require surgery. Follow-up with a specialist is often recommended for an elbow fracture.
Home care
-
Give your child pain medicines as directed by the healthcare provider. Never give aspirin to a child or teen. It could cause a rare but serious condition called Reye syndrome.
-
Follow the healthcare provider's instructions about how much your child should use the affected arm.
-
Keep the child's arm elevated to reduce pain and swelling. This is most important during the first 48 hours after injury. As often as possible, have the child sit or lie down and place pillows under the child’s arm until it's raised above the level of the heart. For infants or toddlers, lay the child down and place pillows under the arm until the injury is raised above the level of the heart. Be sure that the pillows don't move near the face of the infant or toddler. Never leave the child unsupervised.
-
Apply a cold pack to the injury to help control swelling. You can make an ice pack by wrapping a plastic bag of ice cubes in a thin towel. As the ice melts, be careful that the cast or splint doesn’t get wet. Don't place the ice directly on the skin, as this can cause damage. You can place a cold pack directly over a splint or cast.
-
Ice the injured area for up to 20 minutes every 1 to 2 hours the first day. Continue this 3 to 4 times a day for the next 2 days, then as needed. It may help to make a game of using the ice. However, if your child objects, don't force your child to use the ice.
-
Care for the splint or cast as you’ve been instructed. Don’t put any powders or lotions inside the splint or cast. Keep your child from sticking objects into the splint or cast.
-
Keep the splint or cast completely dry at all times. The splint or cast should be covered with 2 layers of plastic, such as 2 plastic bags, and kept out of the water when your child bathes. Close the top end of the bag with tape or rubber bands.
-
Encourage your child to wiggle or exercise their fingers of the affected arm often.
Follow-up care
Follow up with the child's healthcare provider, or as advised. Follow-up X-rays may be needed to see how the bone is healing. If your child was given a splint, it may be changed to a cast at the follow-up visit. If you were referred to a specialist, make that appointment promptly.
Special note to parents
Healthcare providers are trained to recognize injuries like this one in young children as a sign of possible abuse. Several healthcare providers may ask questions about how your child was injured. Healthcare providers are required by law to ask you these questions. This is done for protection of the child. Please try to be patient and not take offense.
Call 911
Call 911 if your child has:
When to seek medical advice
Call your child's healthcare provider right away if any of these occur:
-
Wet or soft splint or cast
-
Splint or cast is too tight (loosen a splint before going for help)
-
Increasing swelling or pain after a cast or splint is put on (nonverbal infants may indicate pain with crying that can't be soothed)
-
Fingers on the injured hand are cold, blue, numb, burning, or tingly
-
Child can’t move the fingers of the affected hand
-
Redness, warmth, swelling, or drainage from the wound, or foul odor from the cast or splint
-
In infants: Fussiness or crying that can't be soothed
-
Fever (see Fever and children, below)
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use a rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below is when to call the healthcare provider if your child has a fever. Your child’s healthcare provider may give you different numbers. Follow their instructions.
When to call a healthcare provider about your child’s fever
For a baby under 3 months old:
-
First, ask your child’s healthcare provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
-
A fever of ___________as advised by the provider
For a child age 3 months to 36 months (3 years):
-
Rectal or forehead: 102°F (38.9°C) or higher
-
Ear (only for use over age 6 months): 102°F (38.9°C) or higher
-
A fever of ___________ as advised by the provider
In these cases:
-
Armpit temperature of 103°F (39.4°C) or higher in a child of any age
-
Temperature of 104°F (40°C) or higher in a child of any age
-
A fever of ___________ as advised by the provider